Homeopathy treatment for Osteoporosis
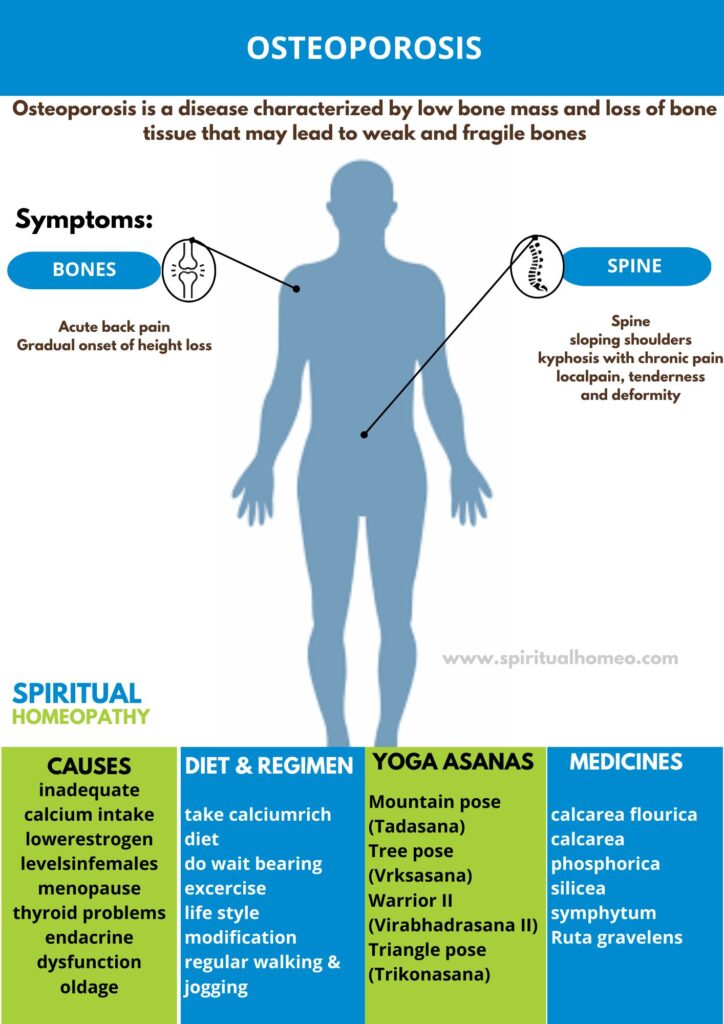
Osteoporosis is a disease characterized by low bone mass and loss of bone tissue that may lead to weak and fragile bones.
- Overview
- Causes
- Types
- Sign & Symptoms
- What to eat
- Diet and Regiment
- Homeopathic Treatment
- FAQ
- Reference
- In general,Osteoporosis is the most common bone disease and affects millions of people worldwide.
- Fractures related to osteoporosis are estimate to affect around 30% of women also 12% of men in developed countries, and are a major public health problem.
- Specifically, In the UK alone, fractures are sustain by over 250000 individuals annually, with treatment costs of about £1.75 billion.
- Osteoporotic fractures can affect any bone, but the most common sites are the forearm (Colles fracture), spine (vertebral fracture) and hip.
- Of these, hip fractures are the most serious.
- Their immediate mortality is about 12% and there is a continue increase in mortality of about 20% when compared with age matched controls.
- All in all, the defining feature of osteoporosis is reduce bone density, which causes a microarchitectural deterioration of bone tissue and leads to an increased risk of fracture.
Prevalence
- The prevalence of osteoporosis increases with age, reflecting the fact that bone density declines with age, especially in women.
Osteoporosis causes bones to become weak and brittle. So brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture.
- Bone is living tissue that is constantly being break down also replace.
Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Osteoporosis occurs when there is an imbalance between new bone formation and old bone resorption.
The body may fail to form enough new bone, or too much old bone may be reabsorbed, or both.
Two essential minerals for normal bone formation are calcium and phosphate. Throughout youth, the body uses these minerals to produce bones.
Calcium:
- It is essential for proper functioning of the heart, brain, and other organs.
- To keep those critical organs functioning, the body reabsorbs calcium that is store in the bones to maintain blood calcium levels.
- If calcium intake is not sufficient or if the body does not absorb enough calcium from the diet, bone production and bone tissue may suffer.
- Thus, the bones may become weaker, resulting in fragile and brittle bones that can break easily.
- Usually, the loss of bone occurs over an extended period of years.
Hormones:
- The leading cause of osteoporosis is a lack of certain hormones, particularly estrogen in women and androgen in men.
- Women, especially those older than 60 years of age, are frequently diagnosed with the disease.
Menopause is accompany by lower estrogen levels and increases a woman’s risk for osteoporosis.
Other factors:
- They may contribute to bone loss in this age group include;
- Inadequate intake of calcium & vitamin D
- Lack of weight-bearing exercise
- Other age-related changes in endocrine functions (in addition to lack of estrogen)
- Overuse of corticosteroids (e.g. Cushing syndrome)
- Thyroid problems
- Lack of muscle use
- Bone cancer
- Certain genetic disorders
- Use of certain medications
- Problems such as low calcium in the diet
Osteoporosis is a condition characterized by weakened bones that are more susceptible to fractures. There are several types of osteoporosis, which are typically classified based on the cause, age of onset, and the underlying factors contributing to bone loss. Below are the primary types of osteoporosis:
1. Primary Osteoporosis
Definition: Primary osteoporosis occurs without any underlying medical conditions or external causes. It is typically related to aging or hormonal changes.
Subtypes:
Type 1 (Postmenopausal Osteoporosis):
Cause: Occurs primarily in women after menopause due to a decrease in estrogen levels, which plays a role in maintaining bone density.
Characteristics: It usually affects trabecular bone (the spongy bone inside the vertebrae and wrists), making bones more porous and susceptible to fractures, especially in the spine and wrist.
Onset: Typically occurs in women aged 50 and older, after menopause.
Type 2 (Senile Osteoporosis):
Cause: Age-related bone loss, which affects both men and women as they get older. It’s related to changes in bone metabolism, including a decline in bone formation and reduced calcium absorption.
Characteristics: This type affects both cortical and trabecular bones and is more common in people aged 70 and older. It is often seen in people who have a long history of low bone mass.
Onset: More common after the age of 70, and both genders are affected, but more frequently in postmenopausal women.
2. Secondary Osteoporosis
Definition: Secondary osteoporosis is a type of bone loss caused by an underlying medical condition, medication, or lifestyle factors.
Causes and Related Conditions:
Medications:
Corticosteroids (Prednisone): Long-term use of corticosteroids is a well-known cause of secondary osteoporosis as they interfere with bone formation and calcium absorption.
Anticonvulsants: Certain medications used for epilepsy (like phenytoin) can impact bone health.
Chemotherapy: Cancer treatments may also affect bone health, especially if used for prolonged periods.
Endocrine Disorders:
Hyperthyroidism: Excessive thyroid hormone can lead to increased bone turnover and loss of bone mass.
Cushing’s Syndrome: High levels of cortisol (from the adrenal glands) can lead to bone loss.
Diabetes: Both Type 1 and Type 2 diabetes can contribute to bone fragility, particularly in those with poorly controlled blood sugar.
Hyperparathyroidism: Overactive parathyroid glands can increase calcium release from bones, leading to bone weakness.
Lifestyle Factors:
Smoking: Smoking accelerates bone loss by reducing blood flow to bones and impairing calcium absorption.
Excessive Alcohol Consumption: Heavy drinking can decrease bone density and increase fracture risk.
Nutritional Deficiencies: Lack of adequate calcium and vitamin D, or eating disorders such as anorexia nervosa, can increase the risk of secondary osteoporosis.
Other Medical Conditions:
Rheumatoid Arthritis: Chronic inflammation from autoimmune diseases can lead to bone loss.
Gastrointestinal Diseases: Conditions like celiac disease or Crohn’s disease, which affect nutrient absorption, can increase the risk of osteoporosis.
Kidney Disease: Chronic kidney disease can result in a loss of calcium and other minerals vital for bone health.
Multiple Myeloma: This bone marrow cancer can cause bone loss, particularly in the spine.
3. Idiopathic Osteoporosis
Definition: Idiopathic osteoporosis refers to cases where the cause of osteoporosis is unknown. This type can occur in younger individuals (both men and women) without any obvious reason or underlying disease.
Onset: It can occur in individuals under the age of 50 and is often discovered when an unusual fracture occurs. In some cases, it may be linked to genetic factors.
4. Juvenile Osteoporosis
Definition: A rare form of osteoporosis that affects children and adolescents, usually due to a genetic or metabolic disorder.
Causes: It may be secondary to conditions like juvenile arthritis or may be idiopathic in nature (without a known cause).
Characteristics: Children with this form of osteoporosis may experience fractures, growth problems, and delayed bone development.
5. Glucocorticoid-Induced Osteoporosis (GIOP)
Definition: A specific form of secondary osteoporosis that occurs as a result of prolonged use of glucocorticoid medications (like prednisone).
Mechanism: Glucocorticoids interfere with bone formation, increase calcium excretion, and can lead to a decrease in bone mass over time.
At Risk: Individuals using glucocorticoids for conditions like rheumatoid arthritis, asthma, lupus, or other autoimmune disorders.
6. Osteoporosis Pseudoglioma Syndrome (OPGS)
Definition: A rare genetic disorder that causes osteoporosis in young individuals. This condition also affects vision and can lead to blindness.
Cause: It’s caused by mutations in the LRP5 gene, which is responsible for bone development. It leads to both weak bones and eye problems, such as a condition called pseudoglioma (an eye condition that can cause blindness).
Patients with osteoporosis are asymptomatic until a fracture occurs.
Osteoporotic spinal fracture may present with;
- Acute back pain
- Gradual onset of height loss
- Sloping shoulders
- Kyphosis with chronic pain.
Acute vertebral fracture:
- It can occasionally radiate to the anterior chest or abdominal wall and mistake for a myocardial infarction or intra abdominal pathology, but worsening of pain by movement and local tenderness both suggest vertebral fracture.
Peripheral osteoporotic fractures:
- It present with local pain, tenderness and deformity, often after an episode of minimal trauma.
Hip fracture:
- The affected leg is shorten and externally rotate.
Diet plays an important role in managing osteoporosis by providing essential nutrients that help maintain strong bones and reduce the risk of fractures. The key nutrients for bone health include calcium, vitamin D, magnesium, protein, and other vitamins and minerals. Here’s a guide to the types of foods you should eat to support bone health if you have osteoporosis:
1. Calcium-Rich Foods
Calcium is one of the most important nutrients for bone health, as it helps maintain bone density and strength. People with osteoporosis need to ensure they’re getting enough calcium to prevent further bone loss.
Dairy Products:
Milk (whole, low-fat, or skim)
Yogurt
Cheese (cheddar, mozzarella, cottage cheese)
Leafy Green Vegetables:
Kale
Collard greens
Spinach (although its calcium may not be as easily absorbed due to oxalates)
Turnip greens
Bok choy
Fortified Foods:
Fortified plant-based milks (almond, soy, oat milk)
Fortified orange juice
Fortified cereals
Fish with Bones:
Sardines
Canned salmon (with bones)
Other Sources:
Tofu (calcium-set)
Almonds
Figs (dried)
2. Vitamin D-Rich Foods
Vitamin D is essential for calcium absorption. Without enough vitamin D, calcium may not be properly absorbed into the bones, which can lead to bone thinning.
Fatty Fish:
Salmon
Mackerel
Sardines
Tuna
Egg Yolks
Eggs provide a moderate amount of vitamin D.
Fortified Foods:
Fortified dairy products (e.g., fortified milk)
Fortified plant-based milk (soy, almond, rice milk)
Fortified cereals
Fortified orange juice
Sunlight:
Sun exposure helps your body produce vitamin D naturally, so try to spend some time outdoors each day, as long as it’s safe to do so.
3. Magnesium-Rich Foods
Magnesium is another mineral that is important for bone health. It helps with the conversion of vitamin D into its active form, which improves calcium absorption.
Nuts and Seeds:
Almonds
Pumpkin seeds
Sunflower seeds
Cashews
Leafy Greens:
Spinach
Swiss chard
Kale
Whole Grains:
Brown rice
Quinoa
Oats
Legumes:
Beans (black beans, kidney beans, chickpeas)
Lentils
Avocados
4. Protein-Rich Foods
Protein is important for overall bone health and helps with the maintenance and repair of tissues. It also contributes to muscle strength, which helps reduce the risk of falls.
Lean Animal Proteins:
Chicken
Turkey
Lean cuts of beef or pork
Fish and Seafood:
Salmon, tuna, and other fatty fish
Plant-Based Proteins:
Tofu
Tempeh
Legumes (lentils, chickpeas, beans)
Nuts and seeds
5. Vitamin K-Rich Foods
Vitamin K plays an important role in bone health by helping with the synthesis of osteocalcin, a protein involved in bone mineralization.
Leafy Greens:
Kale
Spinach
Collard greens
Turnip greens
Swiss chard
Other Vegetables:
Broccoli
Brussels sprouts
Herbs:
Parsley
Basil
6. Phosphorus-Rich Foods
Phosphorus works alongside calcium to help build and maintain bones. It’s essential for bone health, and a good balance of calcium and phosphorus is crucial for strong bones.
Meats:
Chicken
Turkey
Lean cuts of beef
Fish:
Salmon
Mackerel
Tuna
Dairy Products:
Milk
Cheese
Yogurt
Nuts and Seeds:
Almonds
Sunflower seeds
Walnuts
Legumes:
Beans
Lentils
7. Omega-3 Fatty Acids
Omega-3 fatty acids may help improve bone health by reducing inflammation and enhancing bone mineral density.
Fatty Fish:
Salmon
Mackerel
Sardines
Herring
Seeds:
Chia seeds
Flaxseeds
Nuts:
Walnuts
Plant Oils:
Flaxseed oil
Canola oil
8. Anti-Inflammatory Foods
Chronic inflammation can contribute to bone loss. Eating foods with anti-inflammatory properties can help reduce inflammation and support bone health.
Fruits:
Berries (blueberries, strawberries, raspberries)
Cherries
Oranges
Apples
Vegetables:
Leafy greens (spinach, kale)
Tomatoes
Broccoli
Sweet potatoes
Spices:
Turmeric (curcumin)
Ginger
9. Foods to Avoid
While focusing on a bone-healthy diet, there are some foods that can impair bone health or interfere with calcium absorption:
Excessive Salt: High-sodium foods can increase calcium excretion from the body. Limit processed foods, fast food, and high-sodium snacks.
Caffeine: Excessive caffeine can increase calcium loss through urine. Limit coffee and soda consumption.
Alcohol: Heavy drinking can interfere with bone health by reducing bone formation and increasing the risk of fractures.
Sugary Drinks: Sugary sodas and other sweetened beverages may not only be low in nutrients but can also contribute to bone loss.
High-Phytate Foods: Foods high in phytates (such as whole grains, legumes, and nuts) can bind calcium and reduce its absorption. However, the effect is minimal unless they are consumed in large quantities.
Diet for Osteoporosis
A nutrient-dense diet is crucial for supporting healthy bones. Focus on foods that are rich in key nutrients, particularly calcium, vitamin D, magnesium, protein, and vitamin K, all of which play essential roles in bone health.
1. Calcium-Rich Foods (for Bone Strength)
Calcium is a primary building block of bone tissue, and adequate intake is crucial to prevent bone weakening.
Dairy Products: Milk, yogurt, and cheese are excellent sources of calcium.
Leafy Greens: Kale, collard greens, and bok choy are rich in calcium.
Fortified Foods: Many plant-based milks (almond, soy) and orange juice are fortified with calcium.
Fish with Bones: Sardines and canned salmon contain calcium from the bones.
Tofu: Calcium-set tofu is a good source of calcium.
Almonds and Figs: Both are rich in calcium.
2. Vitamin D-Rich Foods (for Calcium Absorption)
Vitamin D is necessary for the absorption of calcium from the digestive tract into the bloodstream.
Fatty Fish: Salmon, mackerel, and sardines are excellent sources.
Egg Yolks: A moderate source of vitamin D.
Fortified Foods: Fortified milk (both dairy and plant-based), fortified cereals, and fortified orange juice.
Sunlight: Vitamin D can be synthesized in the skin when exposed to sunlight. Aim for 10-30 minutes of sun exposure a few times a week, depending on your skin tone and location.
3. Magnesium-Rich Foods (for Bone Metabolism)
Magnesium is essential for bone formation and helps regulate calcium balance.
Leafy Greens: Spinach, kale, and Swiss chard.
Nuts and Seeds: Almonds, sunflower seeds, cashews, and pumpkin seeds.
Whole Grains: Brown rice, quinoa, oats, and barley.
Legumes: Beans, lentils, and chickpeas.
4. Protein-Rich Foods (for Bone and Muscle Health)
Adequate protein supports bone structure, muscle mass, and overall function.
Lean Meat: Chicken, turkey, lean cuts of beef.
Fish: Salmon, tuna, and other fatty fish provide both protein and omega-3 fatty acids.
Plant-Based Proteins: Tofu, tempeh, beans, lentils, and quinoa.
5. Vitamin K-Rich Foods (for Bone Mineralization)
Vitamin K helps with bone mineralization and regulation of calcium.
Leafy Greens: Kale, spinach, and Swiss chard.
Cruciferous Vegetables: Broccoli, Brussels sprouts.
Herbs: Parsley, basil.
6. Omega-3 Fatty Acids (for Bone and Joint Health)
Omega-3 fatty acids help reduce inflammation and support bone health.
Fatty Fish: Salmon, sardines, mackerel.
Nuts and Seeds: Walnuts, flaxseeds, chia seeds.
7. Anti-Inflammatory Foods (for Reducing Bone Loss)
Chronic inflammation can contribute to bone loss, so eating anti-inflammatory foods is beneficial.
Fruits: Berries, oranges, apples, and cherries are rich in antioxidants.
Vegetables: Tomatoes, broccoli, sweet potatoes, and bell peppers.
Spices: Turmeric and ginger have anti-inflammatory properties.
8. Hydration
Drink plenty of water to support overall health, including bone health. Proper hydration helps with nutrient transport and overall bodily functions.
Foods to Avoid for Osteoporosis
Certain foods can interfere with bone health and increase the risk of osteoporosis-related fractures. Limit or avoid:
Excessive Salt: High sodium can lead to calcium loss through urine. Reduce intake of processed foods, canned soups, and salty snacks.
Caffeine: Excessive caffeine intake (more than 3 cups of coffee or 2 sodas a day) can increase calcium loss.
Alcohol: Excessive drinking can disrupt bone formation and decrease calcium absorption.
Soda: Cola beverages contain phosphoric acid, which can interfere with calcium balance.
Sugar: High sugar intake can contribute to bone loss over time.
Regimen for Osteoporosis
A combination of exercise and lifestyle habits is essential for strengthening bones, improving balance, and preventing fractures. It’s important to follow a safe and consistent regimen designed for individuals with osteoporosis.
1. Weight-Bearing Exercises (to Stimulate Bone Growth)
Weight-bearing exercises encourage the bones to build and retain density by placing stress on them.
Walking: One of the simplest and safest weight-bearing exercises.
Jogging: For those without significant joint pain or mobility issues.
Hiking: With natural terrain, hiking offers more variety and challenge.
Dancing: Low-impact dance styles or ballroom dancing can be fun and effective for bones.
Stair Climbing: Encourages bone density and leg strength.
2. Strength Training (to Build Muscle Mass and Support Bones)
Muscle strength helps reduce the load on bones and supports better balance.
Light Weightlifting: Focus on using light weights to avoid overstraining. Dumbbells and resistance bands are great tools.
Resistance Band Exercises: Use bands to provide adjustable resistance for various muscle groups.
Bodyweight Exercises: Squats, lunges, and modified push-ups (if safe to do) strengthen muscles and bones.
3. Balance and Flexibility Exercises (to Prevent Falls)
Improving balance and flexibility can help reduce the risk of falls, which are common in individuals with osteoporosis.
Tai Chi: A gentle, flowing form of exercise that improves balance and flexibility.
Yoga: Focus on gentle poses that stretch muscles and improve bone alignment. Avoid poses that put excessive strain on bones or joints.
Pilates: Helps with flexibility, balance, and core strength.
Standing Balance Exercises: Simple exercises like standing on one leg for a few seconds at a time.
4. Low-Impact Cardiovascular Exercise (for Heart Health and Bone Strength)
Cardiovascular exercises can improve heart health and endurance while being easy on the joints.
Swimming: A great option for low-impact exercise that strengthens muscles and joints without stressing bones.
Cycling: Whether stationary or outdoor, cycling provides cardiovascular benefits while being gentle on bones.
Elliptical Machine: Offers a low-impact alternative to running while still providing an effective cardiovascular workout.
Why Choose Homeopathy?
Homeopathy offers natural and holistic healing, treating the root cause of ailments without side effects. It strengthens the body’s defense system, is gentle for all ages, and personalized to each individual’s needs. Choose homeopathy for safe, effective, and long-lasting health solutions.
Spiritual Homeopathy: Your Path to Natural Healing
At Spiritual Homeopathy, where we believe in the power of holistic healing and personalized care. Our mission is to provide compassionate and effective homeopathic treatment to help you achieve optimal health and well-being. With a focus on addressing the root cause of illness and promoting harmony between mind, body, and spirit, we are dedicated to guiding you on your journey towards vibrant health and vitality.
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs.we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
What is Osteoporosis?
Osteoporosis is a disease characterized by low bone mass and loss of bone tissue that may lead to weak and fragile bones.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Osteoporosis?
- Calcarea Phosphorica
- Calcarea Fluorica
- Silicea
- Symphytum
- Ruta Graveolens
What causes Osteoporosis?
- Calcium intake is not sufficient
- Body does not absorb enough calcium from the diet
- Lack of certain hormones (estrogen)
- They may contribute to bone loss
- Inadequate intake of calcium & vitamin D
- Lack of weight-bearing exercise
- Overuse of corticosteroids
- Thyroid problems
- Lack of muscle use
- Bone cancer
What are the symptoms of Osteoporosis?
- Acute back pain
- Gradual onset of height loss
- Sloping shoulders
- Kyphosis with chronic pain
- Local pain, tenderness and deformity
Reference
- Davidson’s Principles and Practice of Medicine (22nd edition)
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- https://www.medicalnewstoday.com/articles/155646.php
- https://www.emedicinehealth.com/osteoporosis/article_em.htm#are_there_home_remedies_for_osteoporosis
- https://www.womenshealth.gov/a-z-topics/osteoporosis