Diphtheria
Diphtheria is a nasopharyngeal and skin infection caused by Corynebacterium diphtheriae. Toxigenic strains of C. diphtheriae produce a protein toxin that causes systemic toxicity, myocarditis, and polyneuropathy. The toxin is associated with the formation of pseudomembranes in the pharynx during respiratory diphtheria. While toxigenic strains most frequently cause pharyngeal diphtheria, nontoxigenic strains commonly cause cutaneous disease.
- Overview
- Causes
- Types
- Sign & Symptoms
- What to eat
- Diet and Regiment
- Homeopathic Treatment
- FAQ
- Reference
OVERVIEW
While in many regions diphtheria has been controlled in recent years with effective vaccination, there have been sporadic outbreaks in the United States and Europe.
It is still common in the Caribbean, Latin America, and the Indian subcontinent, where mass immunization programs are not enforced. Largescale epidemics of diphtheria have occurred in the post-Soviet independent states. Additional outbreaks have been reported in Algeria, China, and Ecuador.
History
The development of the disease antitoxin in 1898 by von Behring also of the diphtheria toxoid vaccine in 1924 by Ramon led to the near elimination of diphtheria in Western countries. The annual incidence rate in the United States peaked in 1921 at 191 cases per 100,000 populations. In contrast, since 1980, the annual figure in the United States has been. Nevertheless, pockets of colonization persist in North America, particularly in South Dakota, Ontario, and recently the state of Washington. Immunity to diphtheria induced by childhood vaccination gradually decreases in adulthood. In detail; An estimated 30% of men 60–69 years old have antitoxin titers below the protective level. In addition to older age and lack of vaccination, risk factors for diphtheria outbreaks include alcoholism, low socioeconomic status, crowded living conditions, and Native American ethnic background.
Clonally related toxigenic C. diphtheriae strains of the ET8 complex associate with this outbreak. Given that the ET8 complex expressed a toxin against which the prevalent diphtheria toxoid vaccine was effective, the epidemic attribute to failure of the public health infrastructure to effectively vaccinate the population. Socioeconomic instability, migration, deteriorating public health programs, frequent vaccine shortages, delayed implementation of vaccination and treatment in response to cases, also lack of public education and awareness were contributing factors.
CAUSES
Diphtheriae is a gram-positive bacillus that unencapsulated, nonmotile, also nonsporulating. The organism first identified microscopically in 1883 by Klebs and a year later isolated in pure culture by Löffler in Robert Koch’s laboratory. The bacteria have a characteristic club-shaped bacillary appearance and typically form clusters of parallel rays, or palisades, that referred to as “Chinese characters.”
Different Laboratory media
The specific laboratory media recommended for the cultivation of C. diphtheriae rely upon tellurite, colistin, or nalidixic acid for the organism’s selective isolation from other autochthonous pharyngeal microbes. C. diphtheriae may isolated from individuals with both nontoxigenic (tox–) and toxigenic (tox+) phenotypes.
Uchida and Pappenheimer demonstrated that coryne-bacteriophage beta carries the structural gene tox, which encodes diphtheria toxin, also that a family of closely related corynebacteriophages are responsible for toxigenic conversion of tox– C. diphtheriae to the tox+ phenotype. Moreover, lysogenic conversion from a nontoxigenic to a toxigenic phenotype has shown to occur in situ. Growth of toxigenic strains of C. diphtheriae under iron-limiting conditions leads to the optimal expression of diphtheria toxin and believed to a pathogenic mechanism during human infection
TYPES
There are two types: respiratory and cutaneous (skin).
- Respiratory diphtheria
- Respiratory diphtheria presents as a sore throat with low-grade fever and a membrane attached to the tonsils, pharynx, or nose. Neck swelling is usually present in severe disease.
- Respiratory diphtheria can lead to severe breathing problems, heart failure, blood disorders, paralysis, coma and even death.
2. Cutaneous (skin) diphtheria
- In the United States, cutaneous diphtheria, although rare, is most often seen among persons with poor hygiene who live in crowded conditions.
- Skin infections with diphtheria are still common in tropical countries and are even more contagious than respiratory diphtheria.
- Skin wounds are characterized by a scaling rash, sores or by blisters which can occur anywhere on the body. Skin wounds may be painful, swollen and reddened. The skin infection is treated by thorough cleansing with soap and water and appropriate antibiotics.
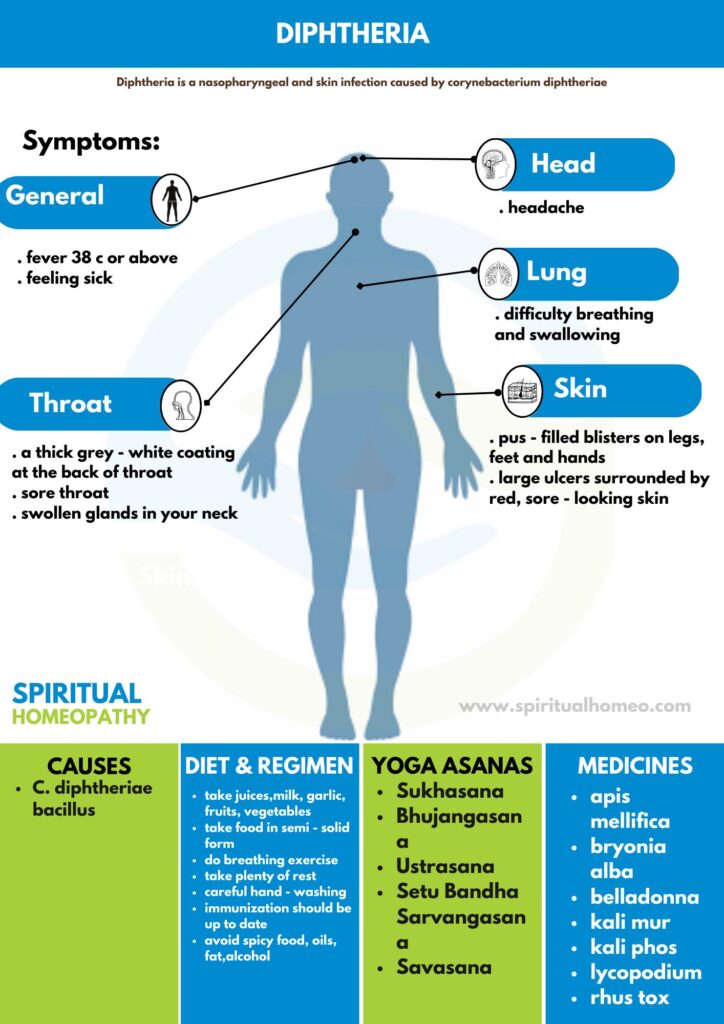
SIGNS AND SYMPTOMS
Symptoms usually start 2 to 5 days after becoming infected.
The main symptoms of diphtheria are:
- A thick grey-white coating at the back of your throat
- A high temperature (in other words; fever) of 38C or above
- Feeling sick
- Sore throat
Headache
- Swollen glands in your neck
- Difficulty breathing and swallowing
If it affects your skin (in other words; cutaneous diphtheria), it can cause:
- pus-filled blisters on your legs, feet and hands
- large ulcers surrounded by red, sore-looking skin
- A patient with diphtheria usually looks ill; systemic signs such as fever, tachypnea, and tachycardia are common. Pharyngeal, respiratory, neurologic, cardiac, and other physical examination findings depend upon the extent and severity of the infection.
WHAT TO EAT
Here’s what to eat for diphtheria, described point-wise:
Hydrating Fluids: Drink plenty of water, herbal teas, and clear broths to stay hydrated and soothe the throat.
Warm Soups: Soft, warm soups can help ease throat pain and provide nutrients without irritating the throat.
Soft, Easily Digestible Foods: Eat soft foods like mashed potatoes, scrambled eggs, and applesauce to avoid irritation.
Vitamin C-rich Foods: Include citrus fruits, berries, and leafy greens to boost immunity and help fight infection.
Honey: Consuming honey can help soothe a sore throat and reduce irritation.
Protein-rich Foods: Include lean proteins like chicken, fish, or tofu to support the immune system and recovery.
Avoid Acidic/Spicy Foods: Stay away from acidic or spicy foods that can irritate the throat and worsen symptoms.
Small, Frequent Meals: Eat small meals throughout the day to maintain energy and avoid overstraining the digestive system.
Always follow medical advice and seek immediate treatment for diphtheria, as it is a serious bacterial infection.
DIET AND REGIMEN
Foods to be taken
- Fluids (e.g. juices)
- Milk
- Garlic
- Food in semi-solid form (e.g. ice creams)
- Fruits and vegetables
Foods to be avoided
- Spicy food
- Oils and fats
- Alcohol
Yoga and Exercise
- Breathing exercise (e.g. pranayama)
- Uttanasana
- Sarvangasana
Home Remedies
- Drink plenty of water
- Take plenty of rest
- Careful hand-washing
- Take diet through liquids and soft foods
- Immunization should be up to date
- Patient should avoid sleeping on their back to steer clear of swallowing the secretion formed in the mouth
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs. we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
FAQ
What is Diphtheria
Diphtheria is a nasopharyngeal and skin infection caused by Corynebacterium diphtheriae. Toxigenic strains of C. diphtheriae produce a protein toxin that causes systemic toxicity, myocarditis, and polyneuropathy
Homeopathic Medicines used by Homeopathic
Doctors in treatment of Diphtheria
- Bryonia Alba
- Belladona
- Lycopodium
- Rhus tox
- Apis mellifica
- Kali Mur
- Arsenicum iod
- Bromium
What causes Diphtheria
Corynebacterium diphtheriae gram-positive bacillus
What are the symptoms of Diphtheria
- A thick grey-white coating at the back of your throat
- A high temperature (fever) of 38C or above
- Feeling sick
- Sore throat
- Headache
- Swollen glands in your neck
- Difficulty breathing and swallowing
REFFERNCE
[1] Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
[2] https://www.mtatva.com/en/disease/diphtheria-treatment-diet-and-home-remedies/
[3] https://www.nhs.uk/conditions/diphtheria/
[4] A Dictionary Of Domestic Medicine By John H.Clarke.
[5]Diphtheria risk factors – wikidoc
[6]Diphtheria – Types, Causes, Symptoms and Prevention. – (diseasesdic.com)
[7]Diphtheria – StatPearls – NCBI Bookshelf (nih.gov)
[8]Diphtheria – Causes, Symptoms, Types, Prevention and Treatments (byjus.com)