Homeopathy treatment for Breast cancer
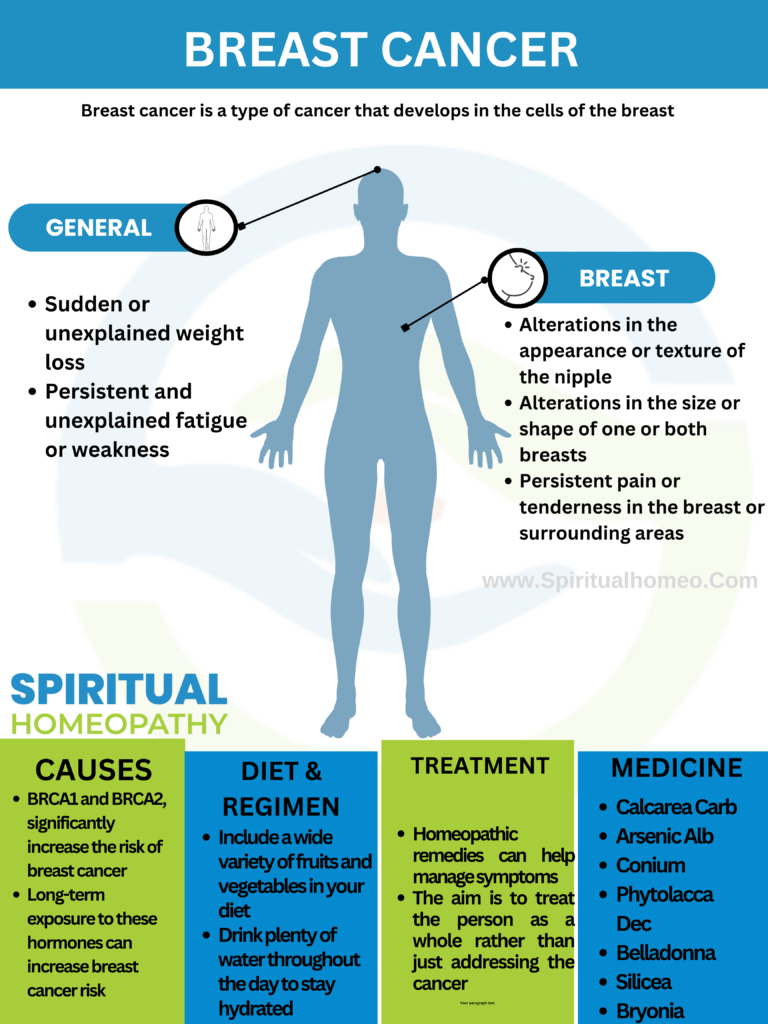
Breast cancer is a type of cancer that originates in the cells of the breast. It occurs when abnormal cells in the breast tissue grow uncontrollably, forming a tumor. If left untreated, breast cancer can spread to other parts of the body
Breast cancer is one of the most common cancers worldwide, primarily affecting women but also occurring in men. It originates in the breast tissue, most commonly in the ducts (which carry milk to the nipple) or the lobules (glands that produce milk). Early detection, advances in treatment, and increased awareness have significantly improved survival rates, making it a critical focus of ongoing research and public health efforts
It seems like you may be referring to “signs and symptoms.” These are two different aspects of how a medical condition presents itself:
Signs
- Definition: Objective evidence of a disease or condition that can be observed or measured by a healthcare provider.
- Examples:
- Fever
- Swelling
- High blood pressure
- Rash
Symptoms
- Definition: Subjective experiences reported by the patient, which cannot be directly observed by others.
- Examples:
- Pain
- Fatigue
- Dizziness
- Nausea
In Context of Illness
- Signs are what the doctor finds during an examination.
- Symptoms are what the patient experiences and reports.
For example, in breast cancer:
- Sign: A doctor might observe a lump in the breast during a physical examination.
- Symptom: The patient might report breast pain or notice changes in breast size.
Understanding both signs and symptoms is crucial for diagnosing and managing medical conditions effectively.
may occur on one side of the lower back, often in advanced stages of the disease.
Breast cancer develops due to a combination of genetic, environmental, and lifestyle factors. While the exact cause of breast cancer is not fully understood, several factors are known to increase the risk of developing the disease:
1. Genetic Factors
- Inherited Gene Mutations: Mutations in certain genes, such as BRCA1 and BRCA2, significantly increase the risk of breast cancer. These mutations can be inherited from either parent.
- Family History: Having close relatives (mother, sister, daughter) with breast cancer increases your risk. A strong family history might indicate the presence of genetic mutations.
2. Hormonal Factors
- Early Menstruation and Late Menopause: Starting menstruation before age 12 or entering menopause after age 55 increases lifetime exposure to estrogen, which can raise breast cancer risk.
- Hormone Replacement Therapy (HRT): Long-term use of HRT, particularly combined estrogen and progesterone therapy, has been linked to an increased risk of breast cancer.
- Birth Control Pills: Some studies suggest a slight increase in breast cancer risk for women using oral contraceptives, though the risk diminishes after stopping the pills.
3. Lifestyle Factors
- Alcohol Consumption: Drinking alcohol is associated with an increased risk of breast cancer, with the risk rising with the amount consumed.
- Obesity and Being Overweight: Especially after menopause, being overweight or obese increases the risk of breast cancer, likely due to higher levels of estrogen produced by fat tissue.
- Lack of Physical Activity: Sedentary lifestyle contributes to obesity, which is a risk factor for breast cancer. Regular exercise can help reduce the risk.
- Diet: High-fat diets and diets low in fruits and vegetables may increase the risk, though evidence is still mixed.
4. Environmental Factors
- Radiation Exposure: Previous exposure to radiation, especially during childhood or adolescence, can increase the risk of breast cancer later in life.
- Exposure to Chemicals: Certain environmental chemicals, such as those found in pesticides or plastics, may have estrogen-like effects that could contribute to breast cancer risk, although research is ongoing.
5. Reproductive History
- First Pregnancy After Age 30 or Never Having Children: Women who have their first full-term pregnancy after 30, or who never have a full-term pregnancy, have a slightly higher risk of breast cancer.
- Not Breastfeeding: Some studies suggest that breastfeeding may slightly lower the risk of breast cancer, especially if done for more than a year.
6. Age and Gender
- Age: The risk of breast cancer increases as you get older, with most cases occurring in women over 50.
- Gender: Being female is the most significant risk factor for breast cancer, though men can also develop the disease, but it is much rarer.
7. Personal History of Breast Cancer or Other Breast Conditions
- Previous Breast Cancer: A woman who has had breast cancer before is at higher risk of developing it again.
- Benign Breast Conditions: Certain non-cancerous breast conditions, like atypical hyperplasia, increase the risk of breast cancer.
8. Dense Breast Tissue
- Women with dense breast tissue (more glandular and fibrous tissue than fatty tissue) are at higher risk because it can make tumors harder to detect and may itself be a risk factor.
9. Ethnicity
- Ethnic Background: Certain ethnic groups, such as Ashkenazi Jewish women, have a higher incidence of BRCA mutations, leading to an increased risk of breast cancer.
10. Other Factors
- Previous Radiation Therapy: Women who had radiation therapy to the chest area (such as for Hodgkin’s lymphoma) before age 30 are at higher risk of developing breast cancer later in life.
Conclusion
While some risk factors, such as genetics and age, cannot be controlled, others, like lifestyle choices, can be managed to reduce the risk of breast cancer. Regular screenings, healthy living, and awareness of family history can also help with early detection and prevention.
Diet plays an important role in supporting overall health during breast cancer treatment and recovery. While no specific food can cure breast cancer, certain foods can help manage side effects, boost the immune system, and support the body’s ability to heal. Here’s a general guide on what to eat if you have breast cancer:
1. Fruits and Vegetables
- Antioxidant-Rich: Include a variety of colorful fruits and vegetables such as berries, oranges, leafy greens, and bell peppers. These are rich in vitamins, minerals, and antioxidants that help protect cells from damage.
- Cruciferous Vegetables: Broccoli, cauliflower, Brussels sprouts, and kale contain compounds like sulforaphane, which may have cancer-fighting properties.
- Fiber-Rich: Whole fruits and vegetables provide fiber, which is essential for digestive health.
2. Whole Grains
- Examples: Brown rice, quinoa, oats, whole wheat, barley, and whole-grain bread and pasta.
- Benefits: Whole grains are rich in fiber, which helps maintain a healthy weight and supports digestion. They also contain essential nutrients like B vitamins and magnesium.
3. Lean Proteins
- Sources: Skinless poultry, fish, eggs, beans, lentils, tofu, and low-fat dairy products.
- Benefits: Protein is crucial for tissue repair and maintaining muscle mass, especially during treatment. Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have anti-inflammatory properties.
4. Healthy Fats
- Sources: Olive oil, avocados, nuts, seeds, and fatty fish.
- Benefits: Healthy fats provide energy, help with the absorption of fat-soluble vitamins (A, D, E, K), and may have anti-inflammatory effects.
5. Foods Rich in Phytoestrogens
- Sources: Flaxseeds, soybeans, tofu, and tempeh.
- Benefits: Phytoestrogens are plant-based compounds that can have a mild estrogen-like effect. While their role in breast cancer is complex, moderate consumption, particularly of soy foods, is generally considered safe and may offer some protective benefits.
6. Hydration
- Water: Staying hydrated is crucial, especially during treatment, as it helps manage side effects like fatigue and constipation.
- Herbal Teas: Ginger tea can help with nausea, and peppermint tea can soothe digestion.
7. Immune-Boosting Foods
- Sources: Garlic, onions, turmeric, ginger, and mushrooms (like shiitake and maitake).
- Benefits: These foods have been shown to support the immune system and may have anti-inflammatory or anti-cancer properties.
8. Probiotic-Rich Foods
- Sources: Yogurt, kefir, sauerkraut, kimchi, and miso.
- Benefits: Probiotics support gut health, which is important for the immune system and digestion, especially during chemotherapy.
9. Limitations and Avoidances
- Limit Processed Foods: Highly processed foods, sugary snacks, and refined grains can contribute to inflammation and weight gain.
- Avoid Excess Alcohol: Alcohol consumption has been linked to an increased risk of breast cancer recurrence.
- Red and Processed Meats: Limit consumption of red meat (beef, pork, lamb) and processed meats (bacon, sausage) due to their potential link to cancer risk.
10. Manage Treatment Side Effects
- Nausea: Eat small, frequent meals, and choose bland foods like crackers, toast, or bananas.
- Fatigue: Opt for energy-boosting foods like complex carbs (whole grains), lean proteins, and healthy fats.
- Mouth Sores: Choose soft, easy-to-chew foods like smoothies, soups, and yogurt.
Conclusion
A balanced diet rich in whole foods, lean proteins, healthy fats, and plenty of fruits and vegetables can support overall health during breast cancer treatment. It’s important to consult with a healthcare provider or a registered dietitian to create a personalized nutrition plan that considers your specific needs and treatment side effects.
1.Radiation Therapy
- External Beam Radiation: The most common type, where high-energy X-rays are directed at the breast from outside the body to destroy cancer cells.
- Brachytherapy (Internal Radiation): Involves placing radioactive seeds or pellets inside the breast tissue near the tumor site.
- Whole-Breast Radiation: Targets the entire breast, often used after a lumpectomy.
- Partial-Breast Radiation: Focuses only on the area where the tumor was removed, reducing radiation exposure to the rest of the breast.
2. Chemotherapy
- Systemic Therapy: Chemotherapy involves using drugs to kill or slow the growth of cancer cells. It can be administered orally or intravenously.
- Neoadjuvant Chemotherapy: Given before surgery to shrink the tumor and make it easier to remove.
- Adjuvant Chemotherapy: Given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Side Effects: Can include fatigue, nausea, hair loss, and increased risk of infection, though these vary depending on the drugs used.
3. Hormone Therapy
- For Hormone Receptor-Positive Cancers: Used to block hormones like estrogen or progesterone that can promote the growth of some breast cancers.
- Tamoxifen: Commonly used for premenopausal and postmenopausal women, it blocks estrogen receptors on breast cancer cells.
- Aromatase Inhibitors (e.g., Anastrozole, Letrozole): Used in postmenopausal women to lower estrogen levels in the body.
- Ovarian Suppression: In premenopausal women, medications or surgery to suppress or remove the ovaries may be used to lower hormone levels.
4. Targeted Therapy
- HER2-Positive Breast Cancer: Some breast cancers have too much of a protein called HER2, which promotes cancer growth. Targeted therapies, such as trastuzumab (Herceptin) and pertuzumab (Perjeta), specifically target these cancer cells.
- CDK4/6 Inhibitors: These drugs, such as palbociclib (Ibrance), help block proteins that promote cancer cell growth and are often used with hormone therapy.
- PARP Inhibitors: For patients with BRCA mutations, drugs like olaparib (Lynparza) may be used to target cancer cells’ ability to repair their DNA.
5. Immunotherapy
- For Triple-Negative Breast Cancer: This approach uses drugs like pembrolizumab (Keytruda) to help the immune system recognize and attack cancer cells. It is typically used in combination with chemotherapy for advanced or metastatic triple-negative breast cancer.
6. Clinical Trials
- Experimental Treatments: Patients may be eligible for clinical trials that test new treatments or combinations of treatments. These trials can provide access to cutting-edge therapies not yet widely available.
7. Supportive and Palliative Care
- Managing Side Effects: Treatments like pain management, nutritional support, and counseling are crucial for maintaining quality of life during and after treatment.
- Palliative Care: For advanced cancer, palliative care focuses on relieving symptoms and improving quality of life, regardless of the stage of the disease.
8. Reconstruction Surgery
- Breast Reconstruction: After a mastectomy, some women choose to have breast reconstruction surgery, which can be done using implants or tissue from another part of the body (autologous reconstruction).
9. Personalized Treatment Plan
- Factors Considered: The treatment plan is personalized based on factors like the type and stage of breast cancer, hormone receptor status, HER2 status, overall health, and patient preferences.
- Multidisciplinary Approach: A team of specialists, including oncologists, surgeons, radiologists, and pathologists, typically collaborates to determine the best treatment plan.
Conclusion
The treatment of breast cancer is complex and tailored to each individual case. Advances in medical research have expanded the range of treatment options, allowing for more personalized and effective care. It’s important for patients to discuss all available options with their healthcare team to make informed decisions about their treatment.
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs.we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
1. What is bladder cancer?
Bladder cancer is a type of cancer that begins in the cells of the bladder, an organ in the lower abdomen that stores urine. The most common type of bladder cancer is urothelial carcinoma, which starts in the cells lining the inside of the bladder.
2. What are the risk factors for bladder cancer?
- Smoking: The most significant risk factor; smokers are several times more likely to develop bladder cancer than non-smokers.
- Age: Most bladder cancers occur in people over 55.
- Gender: Men are more likely to develop bladder cancer than women.
- Exposure to Chemicals: Certain industrial chemicals, such as those used in the dye, rubber, leather, and printing industries, can increase risk.
- Chronic Bladder Infections: Long-term bladder inflammation or infections can raise the risk.
3.What are the common symptoms of bladder cancer?
- Blood in Urine (Hematuria): The most common symptom, which may cause the urine to appear pink, red, or dark brown.
- Frequent Urination: Increased need to urinate, especially at night.
- Painful Urination: Discomfort or pain during urination.
- Lower Back Pain: Pain on one side of the lower back may occur in more advanced stages.
4.How is bladder cancer diagnosed?
- Cystoscopy: A procedure where a thin tube with a camera is inserted through the urethra to view the bladder.
- Urine Cytology: Examining urine under a microscope to look for cancer cells.
- Imaging Tests: CT scans, MRI, or ultrasound may be used to view the bladder and surrounding tissues.
- Biopsy: During cystoscopy, a sample of bladder tissue may be taken to check for cancer cells.
5. What are the stages of bladder cancer?
Bladder cancer is staged based on how far it has spread:
- Stage 0: Cancer is only in the bladder’s inner lining.
- Stage I: Cancer has spread into the bladder wall but not to the muscle layer.
- Stage II: Cancer has spread to the muscle layer of the bladder wall.
- Stage III: Cancer has spread through the bladder wall to surrounding tissues.
- Stage IV: Cancer has spread to nearby organs or distant parts of the body.
1. National Cancer Institute (NCI)
- Website: www.cancer.gov
- Description: Offers comprehensive information on bladder cancer, including treatment options, staging, statistics, and ongoing research.
2. American Cancer Society (ACS)
- Website: www.cancer.org
- Description: Provides detailed guides on bladder cancer, including risk factors, symptoms, early detection, and treatment options.
3. Mayo Clinic
- Website: www.mayoclinic.org
- Description: Offers a broad overview of bladder cancer, including symptoms, causes, diagnosis, and treatment approaches.
4. Bladder Cancer Advocacy Network (BCAN)
- Website: www.bcan.org
- Description: Focuses on bladder cancer awareness, providing resources for patients, caregivers, and healthcare professionals, including support groups and research updates.
5. Urology Care Foundation
- Website: www.urologyhealth.org
- Description: Provides patient-friendly information on bladder cancer, including diagnosis, treatment, and managing side effects.
6. PubMed
- Website: pubmed.ncbi.nlm.nih.gov
- Description: A database of scientific research articles, where you can find peer-reviewed studies and reviews on bladder cancer.
7. World Health Organization (WHO)
- Website: www.who.int
- Description: Offers global perspectives on cancer, including incidence, mortality rates, and prevention strategies, with information specific to bladder cancer.
8. ClinicalTrials.gov
- Website: clinicaltrials.gov
- Description: A registry of clinical trials, where you can find information on ongoing studies related to bladder cancer treatment and management.