Bronchiectasis
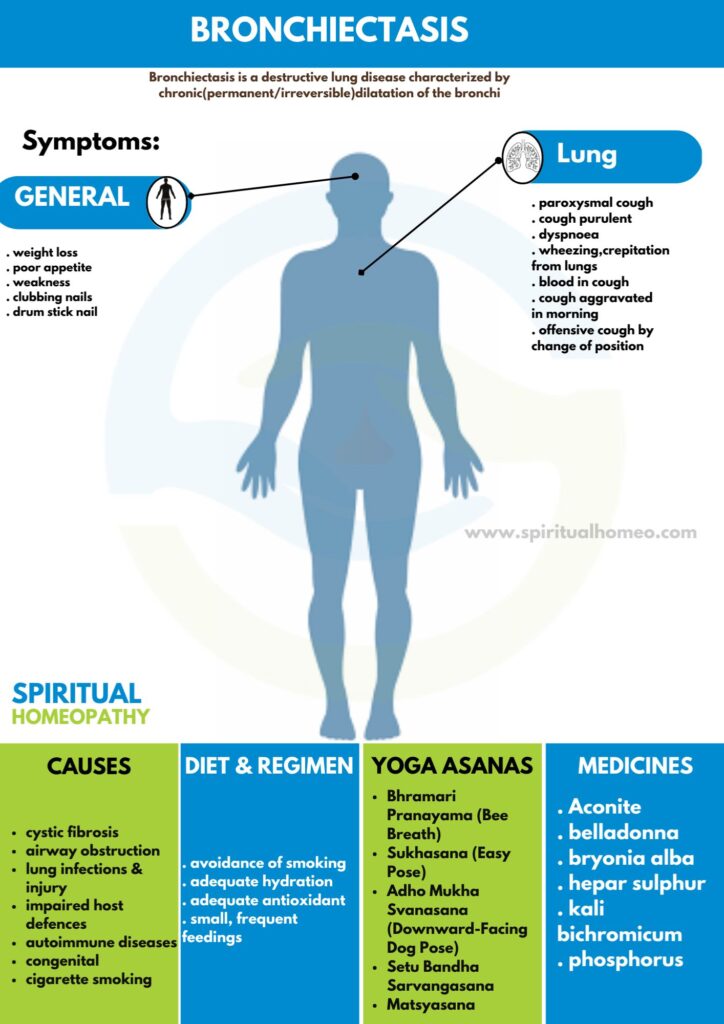
Bronchiectasis a destructive lung disease characterized by chronic (permanent/irreversible) dilatation of the bronchi associated with persistent though variable inflammatory process in the lungs
- Overview
- Causes
- Types
- Sign & Symptoms
- What to eat
- Diet and Regiment
- Homeopathic Treatment
- FAQ
- Reference
OVERVIEW
The disease affects between 1 per 1000 and 1 per 2,50,000 adults. Moreover, the disease is more common in women and increases as people age. Additionally, Cystic fibrosis identify as a cause in up to half of cases.
Bronchiectais without CF is known as non-CFbronchiectasis. Lastly, Historically, about half of all case of non-CFbronchiectasis were found to be idiopathic, or without a known cause.
In detail, there are
CAUSES
In detail, there are many causes that can induce or contribute to the development ofbronchiectasis. The frequency of these different causes varies with geographic location. Additionally, Cystic fibrosis identifies as a cause in up to half of cases.
Bronchiectasis without CF is known as non-CFbronchiectasis. Historically, about half of all case of non-CFbronchiectasis were found to be idiopathic, or without a known cause. However, more recent studies with a more thorough diagnostic work-up have found an etiology in 60 to 90% of patients.
Cystic fibrosis
Cystic fibrosis is the most common life-threatening autosomal recessive disease in the United States and Europe. It is a genetic disorder that affects the lungs, but also the pancreas, liver, kidneys, and intestine. In general, It cause by mutations in the CFTR protein, a chloride channel expressed in epithelial cells. Lung disease results from clogging of the airways due to mucus build-up, decreased muco-ciliary clearance, also resulting inflammation. In later stages, changes to the structure of the lung, such asbronchiectasis, occur. Around 5 to 10% of all patients with cystic fibrosis developbronchiectasis.
Airway obstruction
An airway obstruction can cause by either an intraluminal mass such as a tumor or a foreign body. Furthermore, the presence of an airway obstruction leads to a cycle of inflammation. It is important to identify the presence of an obstruction because surgical resection is often curative if obstruction is the cause. In adults, foreign body aspiration often associate with an altered state of consciousness. The foreign body often unchewed food, or part of a tooth or crown. In conclusion, Bronchiectasis that results from foreign body aspiration generally occurs in the right lung in the lower lobe or posterior segments of the upper lobe.
Lung infections
A range of bacterial, mycobacterial, also viral lung infections are associated with the development ofbronchiectasis. Bacterial infections commonly associated withbronchiectasis i.e. P. aeruginosa, H. influenzae, and S. pneumoniae. Gram-negative bacteria more commonly implicate than gram-positive bacteria. A history of mycobacterial infections such as tuberculosis can lead to damage of the airways that predisposes to bacterial colonization. In brief, Severe viral infections in childhood can also lead tobronchiectasis through a similar mechanism. Nontuberculous mycobacteria infections such as Mycobacterium avium complex found to be a cause in some patients. Lastly, Recent studies have also shown Nocardia infections to implicated inbronchiectasis.
Impaired host defences
Impairments in host defenses that lead tobronchiectasis may be congenital, such as with primary ciliary dyskinesia, or acquired, such as with the prolonged use of immunosuppressive drugs. Additionally, these impairments may localized to the lungs, or systemic throughout the body. In these states of immunodeficiency, there a weakened or absent immune system response to severe infections that repeatedly affect the lung and eventually result in bronchial wall injury. HIV/AIDS an example of an acquired immunodeficiency that can lead to the development ofbronchiectasis.
Aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA) an inflammatory disease caused by hypersensitivity to the fungus Aspergillus fumigatus. It suspected in patients with a long history of asthma also symptoms ofbronchiectasis such as a productive, mucopurulent cough. Imaging often shows peripheral and central airwaybronchiectasis, which unusual in patients withbronchiectasis caused by other disorders.
Autoimmune diseases
Several autoimmune diseases have associated withbronchiectasis. Specifically, individuals with rheumatoid arthritis and Sjogren syndrome have increased rates ofbronchiectasis. In these diseases, the symptoms ofbronchiectasis usually present later in the disease course. Other autoimmune diseases such as ulcerative colitis and Crohn’s disease also have an association withbronchiectasis. Additionally, graft-versus-host disease in patients who have underwent stem cell transplantation can lead tobronchiectasis as well.
Lung injury
It also caused by: inhalation of ammonia and other toxic gases, chronic pulmonary aspiration of stomach acid from esophageal reflux or a hiatal hernia.
CongenitalBronchiectasis
may result from congenital disorders that affect either cilia motility or ion transport. A common genetic cause cystic fibrosis, which affects chloride ion transport. Another genetic cause is primary ciliary dyskinesia, a rare disorder that leads to immotility of cilia and can lead to situs inversus. When situs inversus accompanied by chronic sinusitis andbronchiectasis, this known as Kartagener’s syndrome. Other rare genetic causes include Young’s syndrome and Williams-Campbell syndrome.
Tracheobronchomegaly, or Mourner-Kuhn syndrome a rare condition characterize by significant tracheobronchial dilation and recurrent lower respiratory tract infections. Individuals with alpha 1-antitrypsin deficiency have found to be particularly susceptible tobronchiectasis, due to the loss of inhibition to enzyme elastase which cleaves elastin. This decreases the ability of the alveoli to return to normal shape during expiration.
Cigarette smoking
A causal role for tobacco smoke inbronchiectasis has not demonstrated. Nonetheless, tobacco smoking worse pulmonary function and accelerate the progression of disease that is already present
TYPES
- Cystic fibrosis, which causes almost half of the cases of bronchiectasis in the United States.
- Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
- Allergic bronchopulmonary aspergillosis, which is an allergic reaction to a fungus called aspergillus that causes swelling in the airways.
- Disorders that affect cilia function, such as primary ciliary dyskinesia, can causebronchiectasis. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
- Chronic (long-term) pulmonary aspiration, which can inflame the airways
- Connective tissue diseases, such as rheumatoid arthritis, Sjögren’s syndrome external link, and Crohn’s disease.
SIGNS AND SYMPTOMS
Attacks of recurrent bronchitis, more common in winter. Clubbing of fingers diagnostic.
Hemorrhagic (bronchiectasis sicca) –
Recurrent hemoptysis with good health in-between, or attacks of bronchitis.
Suppurative – For instances; Chronic cough, copious purulent expectoration, general toxemia, clubbing of fingers varying from slight parrot beak curvature of finger nails to bulbous drum stick enlargement (pulmonary osteoarthropathy).
During exacerbations, Dyspnoea and wheezing occur in 75% of patients and pleuritic chest pain in 50%. Pleuritic chest pain cause by distended peripheral airways and inflammation adjacent to the visceral pleura. Pyrexia rare during exacerbations; if it is present, pneumonia should exclude
With relatively rapid onset –
Symptoms developing with comparative suddenness, as a sequel to partial bronchial obstruction by a foreign body or after anesthesia. In early stages paroxysmal cough with occasional offensive sputum which may provoke by change of position. Later large amounts of fetid sputum. Signs mostly limited to auscultation and depend on the size of the affected bronchi, patency of the airways and viscosity of secretions. There may signs of (a) bronchitis, or (b) fibrosis, or (c) consolidation, or (d) collapse, or (e) of cavitation’s.
Early stages –
Fine crackles or sticky rhonchi and slight alteration in character of breath sounds.
Late stages –
Bronchial breathing, coarse crept and perhaps signs of a cavity. Changing character of physical signs after a long bout of cough when air entry may become louder and bronchial in character or from day to day. Sharp metallic or “leathery” rales characteristic. Recurrent pneumonia in the same area of the lung classically associate withbronchiectasis.
WHAT TO EAT
For bronchitis, focus on foods that reduce inflammation, support the immune system, and help with mucus clearance.
- Hydration: Drink plenty of water, herbal teas, or broths to help thin mucus and ease coughing.
- Vitamin C: Consume citrus fruits, strawberries, bell peppers, and broccoli to boost immunity and fight infection.
- Protein: Include lean proteins like chicken, turkey, and legumes to support healing.
- Anti-inflammatory Foods: Add omega-3-rich foods like salmon, flaxseeds, and walnuts to reduce inflammation.
- Garlic and Ginger: These have natural anti-inflammatory and antibacterial properties.
- Avoid Dairy: Dairy may thicken mucus for some people, so it’s best to limit it during flare-ups.
- Whole Grains: Brown rice, oats, and quinoa provide steady energy for recovery.
DIET AND REGIMEN
For bronchiectasis, a diet and regimen that supports lung health and boosts the immune system is key. Here’s a point-wise guide:
- Hydration: Drink plenty of water to thin mucus and aid in easier expectoration.
- Protein-Rich Foods: Include lean proteins (chicken, fish, legumes) to support immune function and muscle strength.
- Antioxidant-Rich Foods: Eat fruits and vegetables (berries, leafy greens, bell peppers) to fight inflammation and support lung health.
- Healthy Fats: Include omega-3s from fish, flaxseeds, and walnuts for anti-inflammatory benefits.
- Limit Salt: Reduce salt intake to help control fluid retention and blood pressure.
- Small, Frequent Meals: Eat small meals to prevent bloating and improve digestion.
- Exercise: Engage in regular, gentle exercise to improve lung function and overall health.
HOMEOPATHYIC TREATMENTS
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs.we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
Homeopathic Remedies for Bronchiectasis
Antimonium Tartaricum: This remedy is often indicated for individuals with bronchiectasis who experience excessive mucus production, rattling cough, and difficulty expectorating mucus. It helps relieve congestion and improve breathing.
Hepar Sulphuris Calcareum: Hepar Sulphuris Calcareum is beneficial for individuals with bronchiectasis who experience chest pain, coughing fits, and sensitivity to cold air. It helps reduce inflammation and promote healing of the bronchial tubes.
Pulsatilla: Pulsatilla is recommended for individuals with bronchiectasis who experience a changeable cough with thick, yellow-green mucus that worsens at night. It helps alleviate coughing spasms and promote expectoration.
Silicea: Silicea is indicated for individuals with bronchiectasis who experience recurrent respiratory infections and weakened immunity. It helps strengthen the immune system and prevent further infections.
Kali Carbonicum: Kali Carbonicum is useful for individuals with bronchiectasis who experience shortness of breath, especially on exertion, and coughing with yellow-green mucus. It helps improve lung function and reduce respiratory symptoms.
Our homeopathic remedies are safe, gentle, and free from side effects, making them suitable for long-term use and individuals of all ages, including children and pregnant women.
Online Consultations with Spiritual Homeopathy
Navigating bronchiectasis can be challenging, but you don’t have to face it alone. At Spiritual Homeopathy, we offer online consultations to provide personalized guidance and support from the comfort of your own home. Our dedicated team of homeopaths will take the time to understand your symptoms, medical history, and emotional state, developing a customized treatment plan tailored to your needs.
During your online consultation, we’ll address your concerns, answer your questions, and recommend the most appropriate homeopathic remedies to promote healing and restore balance. We’ll also provide lifestyle recommendations and self-care strategies to support your overall well-being and enhance the effectiveness of your treatment
FAQ
What is Bronchiectasis?
Bronchiectasis is a destructive lung disease characterized by chronic (permanent/irreversible) dilatation of the bronchi associated with persistent though variable inflammatory process in the lungs.
What are the symptoms of Bronchiectasis?
- Bronchitis- Clubbing of fingers
- Hemorrhagic Hemoptysis
- Suppurative- Chronic cough, Copious purulent expectoration
- Dyspnea and wheezing
- Paroxysmal cough
What are the causes of Bronchiectasis?
- Cystic fibrosis
- Airway obstruction
- Lung infections
- Impaired host defenses
- Aspergillosis
- Autoimmune diseases
- Lung injury
- Congenital
- Cigarette smoking
REFFERNCE
[1] Golwalla’s MEDICINE for Students 25th Edition
[2] Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
[3] Nutrition and Diagnosis-Related Care (Nutrition and Diagnosis-Related Care (Escott-Stump)
[4] https://www.nhlbi.nih.gov/health/bronchiectasis/causes
[5] https://smartvest.com/blog/understanding-types-bronchiectasis/#:~:text=According%20to%20the%20CHEST%20Foundation,cystic%20fibrosis%20bronchiectasis%20(NCFB)
[6] https://bronchiectasis.com.au/assessment/medical/clinical-examination
[7] https://www.google.com/search?q=bronchiectasis+differential+diagnosis&newwindow
[8] https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/treating-and-managing