Homeopathic treatment for Colorectal cancer
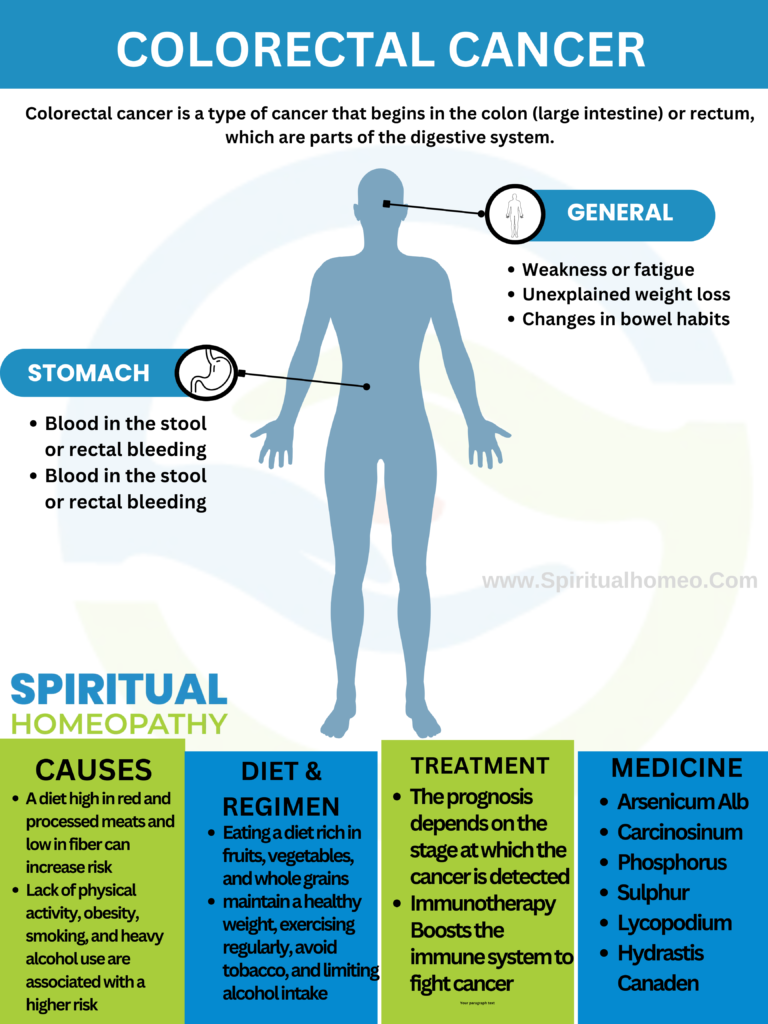
Colorectal cancer is a type of cancer that begins in the colon (large intestine) or rectum, which are parts of the digestive system. The colon and rectum are involved in absorbing water and nutrients from food and storing waste until it is expelled from the body. Colorectal cancer typically starts as a growth called a polyp on the inner lining of the colon or rectum. Over time, some of these polyps can become cancerous.
- Lifestyle Factors: A diet high in red or processed meats, low physical activity, obesity, smoking, and heavy alcohol consumption increase the risk.
- Genetics: Family history of colorectal cancer or inherited syndromes such as Lynch syndrome (hereditary nonpolyposis colorectal cancer) and familial adenomatous polyposis (FAP) significantly increase risk.
- Age: The risk of developing colorectal cancer increases as you age, particularly after age 50.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis are associated with an increased risk.
- Other Factors: Type 2 diabetes, previous radiation therapy to the abdomen or pelvis, and certain racial and ethnic backgrounds (e.g., African Americans and Ashkenazi Jews have higher risks).
Colorectal cancer can develop without any noticeable symptoms, especially in the early stages, which is why regular screening is so important. However, as the disease progresses, certain signs and symptoms may appear. Recognizing these symptoms early can lead to earlier diagnosis and more effective treatment.
Common Signs and Symptoms of Colorectal Cancer:
Changes in Bowel Habits:
- Persistent Diarrhea or Constipation: A noticeable change in bowel habits that lasts more than a few days.
- Narrowing of Stool: Stools that are thinner than usual, sometimes described as “pencil-thin.”
- Incomplete Bowel Movements: A sensation that the bowel doesn’t empty completely, even after a bowel movement.
Rectal Bleeding or Blood in Stool:
- Bright Red or Dark Blood: Blood in the stool can appear bright red or very dark, often making the stool look black or tarry.
- Bleeding with or without Pain: Rectal bleeding may occur without any pain, which can be misleading.
Abdominal Discomfort:
- Cramps or Pain: Frequent abdominal pain, cramping, or discomfort, often described as a persistent ache or bloating.
- Gas and Bloating: Increased gas and bloating that doesn’t go away.
Unexplained Weight Loss:
- Sudden Weight Loss: Losing weight without any change in diet or exercise habits, often a result of the body using more energy to fight the cancer.
- Loss of Appetite: A significant reduction in appetite or feeling full quickly.
Fatigue and Weakness:
- Chronic Fatigue: A feeling of constant tiredness or weakness that doesn’t improve with rest.
- Anemia: Blood loss from rectal bleeding can lead to iron-deficiency anemia, causing fatigue, paleness, and shortness of breath.
Changes in Stool Color or Consistency:
- Unusual Stool Color: Stools may appear very dark or maroon, which can indicate the presence of blood.
- Mucus in Stool: Some people notice mucus mixed in with their stool.
Persistent Urge to Have a Bowel Movement:
- Tenesmus: A continuous feeling that you need to have a bowel movement, even when your bowels are empty.
Symptoms of Advanced Colorectal Cancer:
- Jaundice: Yellowing of the skin and eyes, which can occur if cancer spreads to the liver.
- Breathing Difficulties: If cancer spreads to the lungs, it can cause shortness of breath.
- Bone Pain: Pain in the bones, which can happen if cancer spreads to the bones.
Colorectal cancer, like many other cancers, develops when the cells in the colon or rectum undergo mutations in their DNA, causing them to grow uncontrollably and form tumors. Several factors can increase the risk of these mutations occurring, leading to colorectal cancer. Here are the primary causes and risk factors:
1. Genetic Factors and Family History
Inherited Genetic Mutations: Certain inherited syndromes can significantly increase the risk of colorectal cancer, including:
- Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer or HNPCC): The most common inherited syndrome associated with colorectal cancer, caused by mutations in the DNA mismatch repair genes.
- Familial Adenomatous Polyposis (FAP): A rare, inherited condition where numerous polyps form in the lining of the colon and rectum, with a high likelihood of becoming cancerous if not treated.
- Other Syndromes: MYH-associated polyposis (MAP) and Peutz-Jeghers syndrome are also linked to a higher risk.
Family History: Individuals with a family history of colorectal cancer or adenomatous polyps are at an increased risk, particularly if the relative was diagnosed at a young age.
2. Age
- Increasing Age: The risk of developing colorectal cancer increases significantly with age. Most cases are diagnosed in people over 50, though the incidence in younger adults is rising.
3. Personal History of Polyps or Cancer
- Colorectal Polyps: The presence of adenomatous polyps (precancerous growths) in the colon or rectum increases the risk of colorectal cancer. Although not all polyps become cancerous, most colorectal cancers develop from these types of polyps.
- Previous Cancer: Individuals who have had colorectal cancer or other cancers, such as ovarian, uterine, or breast cancer, have an increased risk of developing colorectal cancer.
4. Inflammatory Bowel Disease (IBD)
- Chronic Inflammation: Long-standing inflammatory bowel diseases like Crohn’s disease and ulcerative colitis are associated with an increased risk of colorectal cancer due to chronic inflammation of the colon.
5. Diet and Lifestyle Factors
- Diet: A diet high in red meat (e.g., beef, pork, lamb) and processed meats (e.g., hot dogs, bacon, sausages) has been linked to an increased risk of colorectal cancer. Cooking meats at high temperatures (frying, grilling) may produce carcinogenic chemicals.
- Low Fiber Intake: A diet low in fruits, vegetables, and whole grains, which are rich in fiber, may increase the risk of colorectal cancer.
- Obesity: Being overweight or obese increases the risk of developing and dying from colorectal cancer. This is particularly true for abdominal obesity.
- Physical Inactivity: Sedentary behavior and lack of regular physical activity are associated with a higher risk of colorectal cancer.
- Smoking: Long-term smokers are more likely to develop colorectal cancer, with the risk increasing with the duration and intensity of smoking.
- Alcohol Consumption: Heavy alcohol use is linked to a higher risk of colorectal cancer, particularly in those who also have other risk factors.
6. Diabetes
- Type 2 Diabetes: Individuals with type 2 diabetes have an increased risk of colorectal cancer, possibly due to insulin resistance and higher insulin levels, which may promote cancer growth.
7. Radiation Therapy
- Previous Radiation Exposure: Radiation therapy directed at the abdomen or pelvis for the treatment of previous cancers (e.g., prostate or cervical cancer) can increase the risk of developing colorectal cancer later in life.
8. Environmental and Occupational Factors
- Occupational Exposure: Exposure to certain chemicals in the workplace, such as those in rubber manufacturing, may increase the risk of colorectal cancer.
- Air Pollution: Some studies suggest that exposure to high levels of air pollution may be linked to an increased risk, although more research is needed to confirm this.
9. Hormonal Factors
- Hormone Replacement Therapy (HRT): Some evidence suggests that postmenopausal women who use hormone replacement therapy may have a slightly increased risk of colorectal cancer, although the data is not conclusive.
10. Microbiome and Gut Health
- Gut Bacteria: The composition of the gut microbiome (the community of bacteria in the intestines) may influence colorectal cancer risk. Certain bacterial imbalances have been associated with increased risk.
Diet plays a crucial role in both the prevention and management of colorectal cancer. If you have been diagnosed with colorectal cancer, eating a balanced and nutritious diet can help support your treatment and recovery. Here are some dietary guidelines and recommendations for individuals with colorectal cancer:
1. High-Fiber Foods
- Whole Grains: Include whole grains like brown rice, whole wheat bread, oats, quinoa, and barley. These foods are high in fiber, which can help maintain regular bowel movements and may reduce the risk of cancer recurrence.
- Fruits and Vegetables: Aim for a variety of colorful fruits and vegetables. They are rich in fiber, vitamins, minerals, and antioxidants that support overall health and may help protect against cancer.
- Examples: Apples, berries, oranges, leafy greens (like spinach and kale), carrots, broccoli, and cauliflower.
2. Lean Proteins
- Poultry and Fish: Opt for lean proteins such as chicken, turkey, and fish. Fatty fish like salmon, mackerel, and sardines are also excellent choices because they are high in omega-3 fatty acids, which may have anti-inflammatory effects.
- Plant-Based Proteins: Include beans, lentils, chickpeas, tofu, and tempeh. These are good sources of protein and fiber without the high fat content of red or processed meats.
3. Healthy Fats
- Olive Oil: Use olive oil as your primary cooking oil. It is a source of healthy monounsaturated fats and antioxidants.
- Nuts and Seeds: Incorporate nuts and seeds like almonds, walnuts, chia seeds, and flaxseeds into your diet. They provide healthy fats and additional fiber.
4. Hydration
- Water: Stay well-hydrated by drinking plenty of water throughout the day. Proper hydration helps with digestion and overall health.
- Herbal Teas: Herbal teas can be a soothing option and provide additional hydration without added sugars.
5. Foods Rich in Antioxidants
- Berries and Citrus Fruits: Berries (such as blueberries, strawberries, and raspberries) and citrus fruits (such as oranges and grapefruits) are high in antioxidants like vitamin C and flavonoids, which may help protect cells from damage.
- Dark Leafy Greens: Spinach, kale, and collard greens are rich in vitamins A, C, and E, as well as folate, which supports cell health.
6. Low-Fat Dairy or Dairy Alternatives
- Low-Fat or Non-Dairy Options: Choose low-fat dairy products like yogurt, cheese, and milk. If you prefer non-dairy options, choose fortified plant-based milks (like almond, soy, or oat milk) that provide calcium and vitamin D.
7. Foods to Limit or Avoid
- Red and Processed Meats: Limit intake of red meats (beef, pork, lamb) and avoid processed meats (such as bacon, sausages, and hot dogs), as they have been linked to an increased risk of colorectal cancer.
- Refined Sugars and Processed Foods: Reduce consumption of foods high in refined sugars (like candy, sugary drinks, and pastries) and highly processed foods, as they can lead to weight gain and do not provide essential nutrients.
- Alcohol: Limit alcohol consumption, as excessive drinking is associated with an increased risk of colorectal cancer. If you choose to drink, do so in moderation.
8. Manage Side Effects of Treatment
- Small, Frequent Meals: Eating smaller, more frequent meals can help manage nausea, loss of appetite, and other side effects of cancer treatment.
- Bland, Easy-to-Digest Foods: If you experience digestive issues, opt for bland, low-fiber foods like white rice, bananas, applesauce, and toast until symptoms improve.
- Probiotics: Consider incorporating probiotic-rich foods like yogurt or kefir to support gut health, especially if you have been on antibiotics.
9. Consult a Dietitian
- Personalized Nutrition Plan: It’s important to consult with a registered dietitian or nutritionist who specializes in oncology to develop a personalized nutrition plan that supports your specific needs during treatment and recovery.
The treatment of colorectal cancer depends on various factors, including the stage of the cancer, the location of the tumor, the patient’s overall health, and personal preferences. Treatment typically involves a combination of chemotherapy, radiation therapy, and targeted therapies. Here’s an overview of the main treatment options:
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop them from growing.
Chemotherapy for Advanced Cancer:
- For metastatic colorectal cancer (cancer that has spread to other organs), chemotherapy can help control the disease and relieve symptoms, though it may not be curative.
Radiation Therapy
Radiation therapy uses high-energy beams, like X-rays, to kill cancer cells.
Palliative Radiation:
- Used in advanced cancer to relieve symptoms such as pain, bleeding, or bowel obstruction.
Targeted Therapy
Targeted therapies are drugs designed to specifically target cancer cells’ genetic mutations or proteins.
Monoclonal Antibodies:
- Bevacizumab (Avastin): Inhibits blood vessel growth in tumors (anti-angiogenesis).
- Cetuximab (Erbitux) and Panitumumab (Vectibix): Target the epidermal growth factor receptor (EGFR), used in some advanced colorectal cancers.
BRAF Inhibitors:
- Used for cancers with a BRAF gene mutation, often combined with other therapies.
Immunotherapy:
- Pembrolizumab (Keytruda) and Nivolumab (Opdivo): Immune checkpoint inhibitors used in some cases of metastatic colorectal cancer, especially those with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR).
Immunotherapy
Immunotherapy helps the immune system recognize and attack cancer cells.
- Checkpoint Inhibitors:
- These drugs, like pembrolizumab and nivolumab, are used particularly in patients with tumors that have specific genetic mutations, such as MSI-H or dMMR.
Palliative Care
For advanced colorectal cancer where cure is not possible, palliative care focuses on relieving symptoms, improving quality of life, and providing support to patients and their families.
- Symptom Management:
- Addressing pain, nausea, fatigue, and other symptoms associated with cancer or its treatment.
- Supportive Therapies:
- Including nutritional support, physical therapy, and psychological counseling.
Clinical Trials
Participation in clinical trials offers access to new and experimental treatments that are not yet widely available.
- Innovative Treatments:
- Clinical trials might include new drugs, combinations of treatments, or advanced techniques like personalized medicine based on genetic profiling.
Follow-Up and Monitoring
Regular follow-up is crucial after treatment to monitor for any signs of recurrence and manage long-term side effects.
- Regular Screening:
- Colonoscopy, imaging tests, and blood tests (like CEA levels) are used to monitor the patient’s condition post-treatment.
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs.we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
FAQ for Colorectal Cancer
1. What is colorectal cancer?
Colorectal cancer refers to cancer that starts in the colon (large intestine) or rectum (the end of the large intestine). It usually begins as small, benign clumps of cells called polyps, which can develop into cancer over time.
2. What are the common symptoms of colorectal cancer?
Symptoms may vary but commonly include:
- Changes in bowel habits (diarrhea, constipation)
- Blood in the stool or rectal bleeding
- Abdominal pain or cramping
- Unexplained weight loss
- Persistent fatigue
- Narrowing of the stool
3. What are the risk factors for colorectal cancer?
Key risk factors include:
- Age (most cases occur in people over 50)
- Family history of colorectal cancer or polyps
- Personal history of polyps or previous cancer
- Inflammatory bowel diseases (e.g., Crohn’s disease, ulcerative colitis)
- Diet high in red or processed meats, low in fiber
- Obesity, physical inactivity
- Smoking and heavy alcohol use
- Certain inherited genetic conditions (e.g., Lynch syndrome, FAP)
4. How is colorectal cancer diagnosed?
Diagnosis typically involves:
- Screening Tests: Colonoscopy, stool tests (like fecal occult blood test), and imaging studies.
- Biopsy: A sample of tissue taken during a colonoscopy to determine if cancer cells are present.
- Imaging Tests: CT scans, MRIs, or PET scans to determine the extent of the cancer and whether it has spread.
5. What are the stages of colorectal cancer?
Colorectal cancer is staged based on how far the cancer has spread:
- Stage 0: Cancer is in the innermost layer of the colon or rectum.
- Stage I: Cancer has grown into the outer layers but has not spread to lymph nodes.
- Stage II: Cancer has spread through the wall of the colon or rectum but not to nearby lymph nodes.
- Stage III: Cancer has spread to nearby lymph nodes but not to distant sites.
- Stage IV: Cancer has spread to distant organs (e.g., liver, lungs).
1. National Cancer Institute (NCI)
- Overview: Comprehensive information on colorectal cancer, including treatment options, risk factors, and ongoing research.
- Website: National Cancer Institute – Colorectal Cancer
2. American Cancer Society (ACS)
- Overview: Detailed resources on colorectal cancer, including statistics, prevention, and treatment.
- Website: American Cancer Society – Colorectal Cancer
3. Mayo Clinic
- Overview: Provides a thorough overview of colorectal cancer, including symptoms, causes, diagnosis, and treatment options.
- Website: Mayo Clinic – Colorectal Cancer
4. Cleveland Clinic
- Overview: Information on colorectal cancer symptoms, diagnosis, and treatment, with guidance on managing the disease.
- Website: Cleveland Clinic – Colorectal Cancer
5. World Health Organization (WHO)
- Overview: Global perspective on colorectal cancer, including statistics, prevention, and health policies.
- Website: World Health Organization – Colorectal Cancer
6. Colorectal Cancer Alliance
- Overview: Support and educational resources for patients, families, and caregivers affected by colorectal cancer.
- Website: Colorectal Cancer Alliance