Homeopathic treatment for piles and haemorrhoid
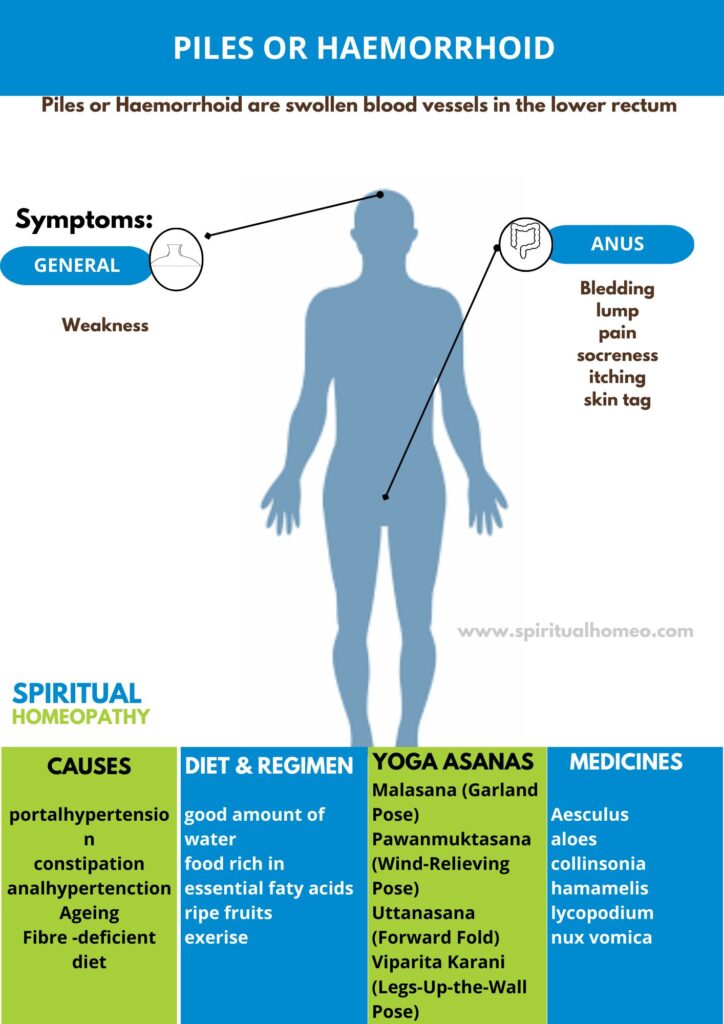
Piles or Haemorrhoid are swollen blood vessels in the lower rectum. Hemorrhoids, also spelled hemorrhoids, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term “hemorrhoid” is often used to refer to the disease.
- Overview
- Causes
- Types
- Sign & Symptoms
- What to eat
- Diet and Regiment
- Homeopathic Treatment
- FAQ
- Reference
Symptomatic hemorrhoids affect >1 million individuals in the Western world per year.
The Prevalence of hemorrhoidal disease is not selective for age or sex. However, Age known to be a risk factor. The prevalence of hemorrhoidal disease less in underdevelope countries.
The typical low-fiber, high-fat Western Diet associate with constipation and straining and the development of symptomatic hemorrhoids.
- Misconceptions concerning the vascular anatomy of the anal canal led to theories of development of primary internal haemorrhoids that lasted for several centuries.
- Man’s upright posture, lack of valves in the portal venous system and raised abdominal pressure were thought to contribute to the development of anal varicosities.
- If raised portal venous pressure were indeed the cause, one would expect a high incidence in subjects suffering from portal hypertension.
- However, although such patients have a higher incidence of anorectal varices, these are a separate anatomical and clinical entity from Haemorrhoid, which are seen no more frequently than in those without cirrhosis, portal hypertension and esophageal varices.
- Other vascular causes Historically, some considered Haemorrhoid to be hemangiomatous or to result from changes in the erectile tissue that forms part of the continence mechanism, such as hyperplasia of the ‘corpus cavernous recti’.
Infection
- Repeated infection of the anal lining, secondary to trauma at defaecation, has been postulated as a cause of weakening and erosion of the walls of the veins of the submucosa.
- This hypothesis is difficult to accept, as one of the truly incredible properties of the anal canal is its resistance to infection, as well as the ability of its mucosa to heal after surgical intervention despite the torrent of micro-organisms passing over it.
Diet and stool consistency
- Much emphasis has been placed on the role of constipation in the development of Haemorrhoid and, indeed, much of the management of sufferers involves attempts to ‘normalize’ bowel habits.
- A fibre-deficient diet results in a prolonged gut transit time, which is associated with the passage of smaller, harder stools that require more straining to expel.
- The presence of a hard Faecal mass in the Rectum could obstruct venous return, resulting in engorgement of the anal veins with the act of straining at stool or sitting for prolonged periods on the lavatory with a relaxed perineum, causing a disturbance of vascular flow.
- However, the epidemiological pattern of constipation is different from that of Haemorrhoidal disease and, indeed, an association has been demonstrated between haemorrhoids and diarrhoeal disorders.
Anal hypertonia
- The association between raised anal canal resting pressure and haemorrhoids is well known, but whether anal hypertonia causes symptoms attributable to haemorrhoids or whether anal cushion hypertrophy causes anal hypertonia is a subject of debate.
- The fact that surgical hemorrhoidectomy restores resting pressures to the normal range is not absolute evidence that the pile masses themselves are the cause of the hypertonia.
- It should be remembered, however, that there are a significant proportion of patients who suffer Haemorrhoidal symptoms in whom the anal canal is relatively patulous, and there is mucosal prolapse, which is associated with perineal descent and pudendal neuropathy.
Ageing
- In contrast to the anal cushion of early life, with age, the supporting structures show a higher proportion of collagen than muscle fibres and are fragmented and disorganised.
- Presumably, these changes arise over time with continued use of the anal canal for defaecation.
- However, similar changes are noted histologically in surgically excised haemorrhoids in younger patients.
- Current view Shearing forces acting on the anus lead to caudal displacement of the anal cushions and mucosal trauma. With time, fragmentation of the supporting structures leads to loss of elasticity of the cushions such that they no longer retract following defaecation.
Classification of Piles or Haemorrhoid
Hemorrhoids are commonly classified as
[1] External
- External Hemorrhoids originate below the dentate line and are covered with squamous epithelium and are associated with an internal component.
- External hemorrhoids are painful when thrombosed.
[2] Internal
- Internal hemorrhoids originate above the dentate line and are Covered with mucosa and transitional zone epithelium and represent majority of hemorrhoids.
- The standard classification of hemorrhoidal disease is based on the progression of the disease from their normal internal location to the prolapsing external position.
External Hemorrhoids
- If not thrombosed, external hemorrhoid may cause few problems.
- However, when thrombosed, hemorrhoids may be very painful.
- Nevertheless, this pain typically resolves in two to three days.
- The swelling may, however, take a few weeks to disappear. A skin tag may remain after healing.
- If hemorrhoids are large and cause issues with hygiene, they may produce irritation of the surrounding skin, and thus itchiness around the anus.
Internal Hemorrhoids
- Internal hemorrhoids usually present with painless, bright red rectal bleeding during or following a bowel movement.
- The blood typically covers the stool is on the toilet paper, or drips into the toilet bowl. The stool itself is usually normally colored.
- Other symptoms may include mucous discharge, a perianal mass if they prolapse through the anus, itchiness, and fecal incontinence.
- Internal hemorrhoids are usually painful only if they become thrombosed or necrotic.
- Bleeding, As the name Haemorrhoid implies, is the principal and earliest symptom. The nature of the bleeding is characteristically separate from the motion and seen either on the paper on wiping or as a fresh splash in the pan.
- Very rarely, the bleeding may sufficient to cause anemia.
- Pain is not commonly associated with the bleeding and its presence should make the clinician alert to the possibility of another diagnosis; however, pain may result from congestion of pile masses below a hypertonic sphincter.
- Piles associated with bleeding Alone call first-degree haemorrhoids.
- Patients may complain of true ‘piles’, lumps that appear at the anal orifice during defaecation and which return spontaneously afterwards (second-degree haemorrhoids), piles that have to replace manually (third-degree haemorrhoids). Or piles that lie permanently outside (fourth-degree haemorrhoids).
- By this stage there is often a significant cutaneous Component to the pile masses, which arise through repeated congestion and Oedema.
- In addition to the main symptoms of pain and prolapse, patients may complain of anal irritation, which may occur as a result of mucus secretion from the caudally displaced rectal mucosa, minor leakage through a now imperfect anal seal or difficulties in cleaning after defaecation because of the irregularity of the anal verge
- Your doctor might be able to see external haemorrhoids. Diagnosing internal haemorrhoids might include examination of your anal canal and rectum.
- Digital examination- Your doctor inserts a gloved, lubricated finger into your rectum. They feels for anything unusual, such as growths.
- Visual inspection- Because internal haemorrhoids are often too soft to be felt during a rectal exam, your doctor might examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
What to Do for Piles (Hemorrhoids)
Hemorrhoids, also known as piles, are swollen blood vessels in the rectum or anus that can cause discomfort, itching, pain, and sometimes bleeding. They are common and can be caused by various factors such as straining during bowel movements, prolonged sitting, pregnancy, or chronic constipation.
Here are some steps you can take to manage and treat hemorrhoids:
1. Dietary Changes:
Increase Fiber Intake: Eating more fiber-rich foods like fruits, vegetables, whole grains, and legumes can help soften stools and reduce straining during bowel movements.
Stay Hydrated: Drinking plenty of water throughout the day helps prevent constipation and ensures the stool remains soft and easy to pass.
2. Over-the-Counter (OTC) Medications:
Topical Creams and Ointments: OTC creams like hydrocortisone or witch hazel can reduce inflammation, itching, and discomfort around the affected area.
Pain Relievers: Oral pain relievers such as acetaminophen or ibuprofen can help alleviate pain and reduce swelling.
Suppositories: Some hemorrhoid creams and suppositories are designed for internal hemorrhoids and can be used for relief.
3. Warm Sitz Baths:
Sitz Bath: Soaking the affected area in warm water for 10-15 minutes several times a day can provide relief from pain and itching. You can do this in a bathtub or use a specially designed sitz bath basin.
4. Avoid Straining:
Don’t Strain During Bowel Movements: Straining puts additional pressure on hemorrhoids, worsening the condition. Go to the bathroom as soon as you feel the urge, and try not to sit on the toilet for long periods of time.
Use a Footstool: Raising your feet on a small stool while sitting on the toilet can help align your body to make bowel movements easier and reduce strain.
5. Proper Hygiene:
Clean Gently: After bowel movements, clean the area with soft, unscented toilet paper, or use wet wipes. Avoid wiping too harshly, as this can irritate the area.
Avoid Scented Products: Don’t use harsh soaps or scented wipes, as they can irritate the hemorrhoids further. Opt for gentle, hypoallergenic products.
6. Exercise:
Regular Physical Activity: Moderate exercise such as walking can help prevent constipation and reduce pressure on hemorrhoids. Avoid activities that put too much strain on the rectal area, such as heavy lifting.
7. Cold Compress:
Apply a Cold Pack: Using a cold compress or ice pack wrapped in a cloth and applying it to the affected area can reduce swelling and numb the pain.
8. Avoid Prolonged Sitting:
Change Positions Regularly: Sitting for long periods can increase pressure on hemorrhoids, so make an effort to stand up and move around at regular intervals, especially if you’re working at a desk or driving for long periods.
9. Medical Treatment for Severe Cases:
If symptoms persist despite home treatments or if the hemorrhoids cause significant bleeding, pain, or other complications, medical treatments may be necessary. These can include:
Rubber Band Ligation: A procedure where a small band is placed around the base of the hemorrhoid to cut off blood supply, causing it to shrink and fall off.
Sclerotherapy: Injection of a solution that causes the hemorrhoid to shrink.
Infrared Coagulation (IRC): Uses infrared light to cut off the blood supply to the hemorrhoid.
Surgical Removal (Hemorrhoidectomy): In extreme cases, surgical removal of hemorrhoids may be necessary.
10. Prevention:
Regular Bowel Movements: Try to avoid constipation and diarrhea by maintaining a healthy diet and lifestyle.
Don’t Ignore the Urge: Respond promptly to the urge to have a bowel movement to avoid straining or prolonged sitting.
When to Seek Medical Attention:
If hemorrhoid symptoms do not improve with self-care.
If you experience significant bleeding.
If there is persistent pain that doesn’t go away.
If you have prolapsed hemorrhoids (hemorrhoids that protrude outside the anus) that are difficult to manage.
A healthy diet and regimen are key in managing and preventing the discomfort and recurrence of piles (hemorrhoids). Below are dietary recommendations and lifestyle changes that can help reduce the symptoms and provide relief:
Dietary Recommendations for Hemorrhoids
Increase Fiber Intake:
Why? Fiber helps soften the stool, making bowel movements easier and reducing the need to strain, which is a major cause of hemorrhoids.
How? Eat fiber-rich foods like:
Whole grains (oats, brown rice, whole wheat bread)
Fruits (apples, pears, berries, bananas)
Vegetables (spinach, kale, broccoli, carrots)
Legumes (beans, lentils, chickpeas)
Nuts and seeds (chia seeds, flaxseeds, almonds)
Hydrate Well:
Why? Drinking plenty of water helps keep stools soft and easy to pass.
How? Aim for 8-10 glasses (about 2-2.5 liters) of water daily. Herbal teas or clear broths can also help maintain hydration.
Avoid Processed and Low-Fiber Foods:
Why? Low-fiber foods (like white bread, refined cereals, and fast food) can lead to constipation and make hemorrhoids worse.
How? Limit or avoid processed foods, sugary snacks, and refined grains. Focus on whole foods that provide natural fiber.
Include Healthy Fats:
Why? Healthy fats lubricate the digestive system and can help ease bowel movements.
How? Include sources of healthy fats in your diet, such as avocados, olive oil, nuts, and fatty fish (like salmon and mackerel).
Incorporate Probiotics:
Why? Probiotics support gut health and can help maintain regular bowel movements.
How? Include probiotic-rich foods such as yogurt, kefir, kimchi, and sauerkraut in your diet.
Limit Caffeine and Alcohol:
Why? Both caffeine and alcohol can dehydrate the body, leading to harder stools and constipation.
How? Cut down on caffeinated drinks (coffee, soda, energy drinks) and alcohol. If consumed, make sure to drink plenty of water alongside.
Avoid Excessive Salt:
Why? Too much salt can cause water retention and swelling, which may worsen hemorrhoid symptoms.
How? Limit high-sodium foods like processed meats, chips, and salty snacks.
Daily Regimen for Hemorrhoids
Regular Exercise:
Why? Physical activity promotes regular bowel movements and improves circulation, reducing pressure on hemorrhoids.
How? Aim for at least 30 minutes of moderate exercise (like walking, swimming, or cycling) most days of the week. Avoid activities that involve heavy lifting or prolonged sitting.
Avoid Prolonged Sitting:
Why? Sitting for long periods, especially on the toilet, can put extra pressure on hemorrhoids.
How? Take breaks if you’re sitting for long stretches, especially when working or driving. Stand up, stretch, and move around every 30-60 minutes.
Practice Proper Toilet Habits:
Why? Straining during bowel movements can aggravate hemorrhoids.
How?
Go to the bathroom as soon as you feel the urge.
Don’t sit on the toilet for long periods (avoid reading or using your phone while on the toilet).
Consider using a footstool to elevate your feet while sitting on the toilet; this helps align your body and reduces straining.
Warm Sitz Baths:
Why? Soaking in warm water can help soothe irritation and reduce inflammation.
How? Sit in a warm bath for 10-15 minutes a few times a day, particularly after bowel movements, to relieve pain and itching.
Good Hygiene Practices:
Why? Cleanliness is important to prevent further irritation and infection.
How? Gently clean the area with moist wipes or soft toilet paper after bowel movements. Avoid using scented or harsh products that could irritate the area.
Use Gentle, Unscented Wipes: Instead of toilet paper, you can use hypoallergenic, fragrance-free wipes, which are gentler on the sensitive skin around hemorrhoids.
Topical Treatments:
Why? Creams and ointments can help reduce swelling, pain, and itching.
How? Apply over-the-counter hemorrhoid creams or ointments containing hydrocortisone or witch hazel to the affected area. Make sure to follow the instructions carefully.
Cold Compress:
Why? Applying cold helps reduce swelling and provides relief from pain.
How? Use a cold compress or ice pack wrapped in a cloth and apply it to the affected area for a few minutes at a time.
Avoid Lifting Heavy Objects:
Why? Lifting heavy items can increase pressure in the rectal area, worsening hemorrhoids.
How? If possible, avoid heavy lifting, and practice good body mechanics when you need to lift something.
Why Choose Spiritual Homeopathy?
At Spiritual Homeopathy, we offer a unique approach to healing that integrates traditional homeopathic principles with a deep understanding of the spiritual aspects of health. Our team of experienced homeopathic practitioners combines expertise with empathy, ensuring that you receive the highest standard of care tailored to your individual needs.
Our Approach to Treatment
We believe that true healing occurs when all aspects of a person—physical, emotional, and spiritual—are in balance. That’s why our treatment approach goes beyond simply addressing symptoms to identify and treat the underlying imbalances contributing to your health concerns. By addressing the root cause of illness and supporting your body’s innate healing ability, we empower you to achieve lasting health and vitality.
Services We Offer
Consultations: Our experienced best homeopathy doctors in Hyderabad offer comprehensive consultations to assess your health concerns, medical history, and individual needs.we also take online consultation and We take the time to listen to your story, understand your unique health goals, and develop personalized treatment plans tailored to your specific needs.
Remedies: At Spiritual Homeopathy, we provide a wide range of homeopathic remedies carefully selected to address a variety of health conditions. From acute ailments to chronic diseases, our remedies are safe, gentle, and effective, offering natural relief without the side effects often associated with conventional medications.
Follow-Up Care: We believe in the importance of ongoing support and monitoring throughout your healing journey. Our team is dedicated to providing regular follow-up care to track your progress, adjust treatment as needed, and ensure that you are on the path to optimal health and well-being.
Our Commitment to You
At Spiritual Homeopathy, your health and wellness are our top priorities. We are committed to providing you with compassionate care, personalized treatment, and the support you need to achieve your health goals. Whether you are seeking relief from a specific health concern or simply looking to optimize your overall well-being, we are here to support you every step of the way.
What causes Piles?
- Portal hypertension and varicose veins
- Infection
- Diet and stool consistency
- Anal hypertonia
- Ageing
What are the symptoms of Piles?
- Painful
- Pain typically resolves in two to three days
- Swelling
- Mucous discharge
- Perianal mass if they prolapse through the anus
- Itchiness
- Fecal incontinence
conditions/hemorrhoids/diagnosis-treatment/drc-20360280
Reference
[1]Harrisons_Principles_of_Internal_Medicine_19th_Edition-_2_Volume_Set
[2] Therapeutics from Zomeo Ultimate LAN
[3] Bailey_and_Love_s_Short_Practice_of_Surgery